Table of Contents
I. Type 1 and Type 2 Diabetes Defined
II. Type 1 vs Type 2 Diabetes: Key Differences
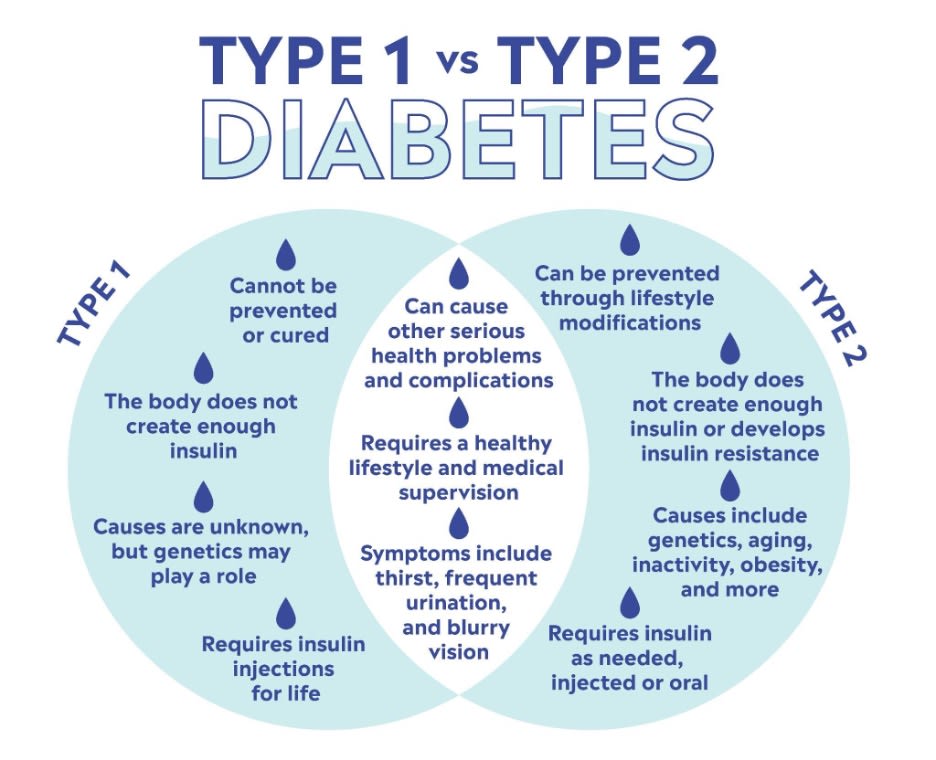
Diabetes now affects more than 500 million people globally, making it one of our world’s most significant health challenges. [1] It primarily manifests in type 1 and type 2, each of which has its own pathophysiology and management requirements. Understanding type 1 vs. type 2 diabetes is crucial for effective diabetes management.
Type 1 diabetes, often diagnosed in children and young adults, is an autoimmune condition where the pancreas produces little to no insulin. Type 2 diabetes is more prevalent in adults, arising from the body's inability to use the insulin it produces effectively.
In this article, we’ll deep-dive into both types, their key differences, and what those differences mean for patient health, medications, treatment plans, and long-term prognosis.
Quick Takeaways:
- Type 1 diabetes is an autoimmune condition that requires insulin management, typically diagnosed in younger individuals.
- Type 2 diabetes develops primarily due to lifestyle factors and genetic predispositions, often diagnosed in adults but increasingly in younger people.
- The management of Type 1 diabetes involves constant insulin use, whereas Type 2 can often be managed initially through lifestyle changes and may later require medication.
- Early diagnosis and tailored treatment strategies are critical for both types of diabetes to prevent complications and manage the disease effectively.
- Continuous education and dialogue with healthcare providers help individuals navigate their treatment options and enhance their quality of life.
Type 1 and Type 2 Diabetes Defined
Type 1 and type 2 diabetes each arise from different pathological processes, impact patients differently, and require specific management strategies. Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This type of diabetes is typically diagnosed in children and young adults.
Due to the body’s inability to produce insulin, individuals with Type 1 diabetes are dependent on insulin injections or pumps to manage their blood glucose levels. The onset of Type 1 diabetes is usually rapid, and its symptoms can quickly become severe. These symptoms often include increased thirst, frequent urination, hunger, weight loss, and fatigue.
Type 2 Diabetes is more common and usually develops in adults over the age of 45, but it is increasingly occurring in younger age groups, including adolescents, children, and even infants. It is characterized by insulin resistance, where the body's cells do not respond properly to insulin. Over time, the pancreas cannot make enough insulin to overcome this resistance. Factors like obesity, physical inactivity, and poor diet are strongly linked to its development.
Symptoms of Type 2 diabetes develop more gradually and include similar signs as type 1, such as thirst and frequent urination, as well as blurred vision and slow healing of wounds.
Both type 1 and type 2 diabetes involve blood sugar regulation, but their underlying mechanisms and management strategies differ significantly. Getting a proper diagnosis is crucial for effective management and treatment, which must be tailored to the specifics of each type.
Type 1 vs Type 2 Diabetes: Key Differences
A clear understanding of type 1 vs. type 2 diabetes is essential for patients to fully have a grasp on their condition, how to manage it, and its full health implications. In this section, we’ll outline some of the aforementioned differences in more detail and explore additional factors that distinguish the two types from each other.
1. Cause
Type 1 diabetes is primarily an autoimmune disease where the body’s immune system attacks its insulin-producing cells in the pancreas. Type 2 diabetes, on the other hand, is influenced by lifestyle factors and genetics, leading to insulin resistance and eventually decreased insulin production.
2. Age of Onset
Type 1 diabetes typically manifests at a young age, often in children and teenagers. Type 2 diabetes usually develops in adults over the age of 45, although it is now increasingly being diagnosed in younger populations due to rising obesity rates.
3. Management
Management of Type 1 diabetes always involves insulin therapy, as the body cannot produce insulin on its own. Type 2 diabetes management may start with lifestyle modifications such as diet changes and exercise; however, medications and possibly insulin therapy may be required as the disease progresses.
4. Progression of the Disease
Type 1 diabetes generally has a rapid onset, with symptoms developing over a short period of weeks to months. In contrast, Type 2 diabetes progresses gradually, and symptoms may not be apparent until the disease is significantly advanced.
5. Symptoms
The initial symptoms of Type 1 diabetes are often severe and sudden, including excessive thirst, frequent urination, hunger, fatigue, and weight loss. For type 2 diabetes, symptoms may be milder initially, such as slight fatigue, more gradual weight gain, and more frequent infections.
6. Risk Factors
The risk factors for Type 1 diabetes are less understood but include genetic predisposition and possibly environmental factors like viral infections triggering autoimmune responses. Risk factors for Type 2 diabetes are more defined, with obesity, poor diet, physical inactivity, and a family history of diabetes identified as the most significant.
7. Diagnosis and Treatment
The diagnosis of Type 1 diabetes typically occurs after symptoms become evident and is confirmed through blood tests that measure blood glucose levels, A1C, and sometimes the presence of autoantibodies. For Type 2 diabetes, diagnosis might result from routine screening before symptoms have fully developed, especially in individuals with risk factors like obesity and family history.
Treatment for Type 1 diabetes invariably involves insulin therapy, which may be administered through injections or a pump to mimic the body’s natural insulin production. Type 2 diabetes treatment often begins with lifestyle modifications—such as diet, exercise, and weight management—and may include oral medications to improve insulin sensitivity or secretion. Over time, some individuals with Type 2 diabetes may require insulin
8. Monitoring
Continuous monitoring of blood glucose levels is essential for both types of diabetes, but the approach can differ. Individuals with Type 1 diabetes frequently use continuous glucose monitors (CGMs) or regular finger-stick testing to manage insulin therapy accurately. In contrast, those with Type 2 diabetes might not progress to frequent blood glucose testing until medication or insulin becomes necessary.
Wrapping Up
Managing diabetes requires medical intervention and a commitment to ongoing education and self-care. By understanding the nuances between type 1 vs. type 2 diabetes, individuals can take active steps towards better health outcomes. Education about the condition empowers patients to make informed decisions about their health that can significantly improve their quality of life.
If you’re affected by diabetes or at risk of developing it, continue learning about the condition and seek out resources that can help. Remember, managing diabetes is a lifelong journey that involves adapting to changes in your health needs.
My Drug Center can be a resource for safe, affordable, and convenient access to important diabetes medications. Visit our website to learn more about how we help maximize medication accessibility with affordable prices and at-home delivery.
The information in the article is not meant to be used for treatment or diagnosis. It is designed for general awareness and for information purposes only. Always consult a medical professional for your specific healthcare needs.
